- +971 50 700 5472
- info@tamphysioandrehab.com
- Crystal Plaza Majaz Sharjah UAE
Tam Physio & Rehabilitation Medicine Most Common Musculoskeletal Pathologies
We treat most common MSK- Conditions under supervision of MOH Certified Physiotherapists & TCAM Practitioners

Piriformis Syndrome: A Complete Guide from Diagnosis to Active Management
Understanding Piriformis Syndrome
Piriformis syndrome is a neuromuscular condition characterized by sciatic nerve entrapment at the level of the piriformis muscle in the buttock. This deep muscle, which helps rotate the hip, lies in close proximity to the sciatic nerve. When the piriformis muscle becomes irritated, inflamed, or goes into spasm, it can compress or irritate the adjacent sciatic nerve, leading to pain, tingling, and numbness that often radiates down the leg.
While the symptoms mimic sciatica, the source is muscular rather than spinal. It is estimated to be responsible for 0.3% to 6% of all cases of low back pain and/or sciatica.
Causes and Contributing Factors
The syndrome typically arises from conditions that cause the piriformis muscle to impinge on the sciatic nerve. These can be categorized as follows:
Muscle Dysfunction:
Spasms, tightening, hypertrophy (enlargement), or inflammation of the piriformis muscle.
· Trauma or Injury: A direct fall onto the buttocks, hip injury, or a sudden, forceful internal rotation of the hip.
· Lifestyle and Overuse: Prolonged sitting (common in office workers or drivers), repetitive activities like long-distance running, or climbing stairs with poor form.
· Anatomical Variations: In some individuals, the sciatic nerve passes through the piriformis muscle instead of beneath it, making them more susceptible to compression.
Who is Commonly Affected?
Piriformis syndrome is most frequently seen in middle-aged adults. Epidemiological data indicates it affects women more often than men, with a reported ratio of 1:6. It is also commonly seen in athletes during periods of intense conditioning and individuals with sedentary occupations.
Clinical Symptoms
Patients typically experience symptoms in the buttock, hip, and upper leg, which may radiate down the back of the thigh. Common descriptions include:
· Pain: A dull ache, burning, or shooting pain in the buttock.
· Radiating Sensations: Tingling, numbness, or "pins and needles" that travel down the back of the thigh, calf, and sometimes into the foot.
· Aggravating Factors:
Symptoms often worsen with activities that engage the muscle, such as:
· Sitting for prolonged periods (especially on hard surfaces).
· Walking, running, or climbing stairs.
· Getting out of bed.
· Relieving Factors: Symptoms may feel better when lying on the back.
Posture, Gait, and Physical Examination
Diagnosis is primarily clinical, involving a history review and physical exam to rule out other conditions like lumbar disc herniation.
Observation:
A clinician may observe altered gait or posture, such as a slight limp or an aversion to sitting squarely on the affected side.
Palpation: Deep palpation of the buttock near the sciatic notch often reveals tenderness over the piriformis muscle belly.
Special Diagnostic Tests
Several provocation tests are used to reproduce symptoms by stretching or contracting the irritated piriformis muscle.
· FAIR Test: The primary clinical test. The patient lies on their back while the examiner flexes, adducts, and internally rotates the hip. Reproduction of pain is a positive sign.
· Freiberg Sign: The examiner forcefully internally rotates the patient's extended thigh.
· Pace Test: The patient resists abduction and external rotation of the thigh while seated.
· Beatty Maneuver: While lying on the unaffected side, the patient holds their flexed knee a few inches off the table, producing deep buttock pain.
Piriformis Syndrome vs. Lumbar Disc Herniation
While both can cause sciatica,key differences help guide diagnosis:
Primary Symptom Location:
· Piriformis Syndrome: Buttock-focused pain
· Lumbar Disc Herniation: Lower back and leg pain
Presence of Back Pain:
· Piriformis Syndrome: Minimal or none
· Lumbar Disc Herniation: Common and often severe
Leg Weakness/Numbness:
· Piriformis Syndrome: Less common
· Lumbar Disc Herniation: More common
Tight Piriformis Muscle:
· Piriformis Syndrome: Hallmark finding
· Lumbar Disc Herniation: May or may not be present
Therapeutic Massage and Trigger Point Therapy
Massage is a core component of conservative treatment, aimed at relaxing the muscle, improving blood flow, and relieving nerve compression.
· General Therapeutic Massage:
Deep tissue massage helps stretch, loosen, and elongate the tight piriformis muscle, improving pain and function.
· Trigger Point Therapy (Neuromuscular Therapy): This specialized technique involves applying sustained pressure for 30 seconds to 2 minutes on specific "knots" or trigger points within the piriformis muscle. This pressure helps release contracted muscle fibers and alleviate pain.
· Self-Massage Techniques:
· Foam Rolling: Lying on a foam roller placed under the buttock and gently rolling can provide myofascial release.
· Tennis/Lacrosse Ball: Sitting or lying on a ball placed under the tender area of the buttock allows for more targeted, sustained pressure on trigger points.
Adopting an Active Lifestyle and Preventive Measures
Long-term management focuses on activity modification, strength, and flexibility.
1. Correct Daily Habits:
· Sitting: Use an ergonomic chair, keep feet flat, and take standing breaks every 30-45 minutes.
· Posture: Maintain a straight back with shoulders relaxed and core engaged. Avoid crossing legs.
· Lifting: Bend at the knees, keep objects close to your body, and avoid twisting.
2. Incorporate Strategic Stretching:
Daily stretching is crucial.Effective stretches include the supine piriformis stretch (figure-four stretch), seated spinal twists, and the standing step-behind piriformis stretch.
3. Engage in Safe, Supportive Exercise:
· Low-Impact Aerobics: Activities like walking, stationary biking, swimming, or water aerobics maintain fitness without excessive strain.
· Strengthening: Focus on building strength in the core, glutes, and hip stabilizers to reduce undue load on the piriformis.
· Proper Warm-Up/Cool-Down: Always prepare muscles for activity and aid recovery afterward.
4. Use Heat and Cold Therapy:
· Cold Packs: Apply for 15 minutes to reduce acute inflammation and pain.
· Heat Therapy: Use a heating pad to relax a tight muscle and improve blood flow before stretching.
When to Seek Professional Care
Consult a healthcare provider—such as a primary care doctor, physical therapist, or orthopedic specialist—if:
· Pain follows an injury or lasts more than a few weeks despite self-care.
· You experience sudden weakness, numbness in the leg, or loss of bowel/bladder control.
· Pain is severe and unrelenting.
Most cases resolve with conservative treatment, including rest, physical therapy, and the measures outlined above. Medical interventions like steroid injections or, very rarely, surgery are considered only if conservative measures fail.
Are You Suffering from Knee Pain During Prayer
Osteo-arthritis of Knee
If you’re over 40 and notice your knees ache, your body shape is changing, and activity feels harder, this message is for you. You might be on a path so many unknowingly walk—towards osteoarthritis of the knee, often ending in a surgeon’s recommendation for knee replacement. But this journey is not inevitable. It’s often the result of neglected health awareness and a misunderstanding of how our bodies change.
The Silent Progression:
From Fat to Weakness to “Bone-on-Bone”
It often starts subtly:
1. Weight Creep & Body Reshaping: We neglect rising body weight. Excess fat first deposits around the flanks (love handles) and abdomen.
2. Fat Replaces Muscle: This fat doesn’t just sit under the skin; it infiltrates muscle tissue, weakening our most important shock absorbers—the thigh muscles (quadriceps and hamstrings).
3. The Knee Bears the Burden:
Weaker muscles mean the knee joint loses stability and cushioning. The load shifts directly onto the cartilage.
4. The Inevitable Conclusion:
Years of this stress wear down the protective cartilage until it’s “bone-on-bone.” Pain becomes severe, and a knee replacement can appear as the only solution.
This creates a cycle that fuels a billion-dollar global industry. While surgery is a genuine lifesaver for advanced cases, the focus must shift dramatically to prevention and early action.
Your Early Warning Signs: Don’t Ignore These!
Your body sends signals long before severe damage. Heed them:
· Early Knee Pain: Stiffness in the morning or after sitting, aching during or after walking/using stairs, pain when kneeling or squatting.
· Muscle Weakness Clues: Trouble rising from a chair without using your arms, feeling unsteady going downstairs, noticing your thighs look softer, less toned even if the scale hasn’t moved drastically (a sign of muscle loss and fat infiltration).
· Body Shape Alert: An increasing waistline and thickening thighs are not just cosmetic issues. They are direct indicators of metabolic and muscular decline that targets your knees.
The Powerful Alternative: Start in Your Early 40s
This is the most critical decade for intervention. Your 40s are when you can truly alter the trajectory of your joint health.
1. Track More Than Weight: Monitor your waist circumference and body composition. Aim to preserve and build muscle mass.
2. Nourish to Protect:
Anti-inflammatory foods (fruits, vegetables, nuts, fish), lean protein for muscle repair, and calcium/Vitamin D for bone health. Limit junk food that accelerates inflammation and fat gain.
3. Build an Active Lifestyle:
· Strength Train: This is non-negotiable. Squats, lunges, leg presses (with proper form) rebuild the quadriceps and hamstrings, creating a “natural brace” for your knee.
· Low-Impact Cardio:
Walking, cycling, and swimming maintain fitness without pounding your joints.
· Stay Flexible: Regular stretching or yoga maintains range of motion.
The Call to Action: For Doctors & Patients
To surgeons and physicians: Let’s stress prevention with the same urgency as surgical solutions. Prescribe nutrition and exercise plans as proactively as we prescribe painkillers.
To every individual: See your body as a system. Your knee pain is not an isolated issue—it’s linked to your muscle health, your weight, and your daily habits.
Don’t wait for the joint to fail. Empower your muscles, manage your weight, and invest in an active lifestyle
Disclaimer:
This is for health awareness only. If you are experiencing these symptoms, please consult a healthcare professional (like a doctor, physiotherapist, or chiropractor) for an accurate diagnosis and a personalized treatment plan.starting today. Your knees are meant to last a lifetime—with care, they can.

Are You Suffering from Lower Back Pain
The sacroiliac (SI) joints are the sturdy connections between your spine (sacrum) and your pelvis (ilium). While designed for stability, they can become a source of significant pain and dysfunction. Let's break down what SI Joint Dysfunction is, how to recognize it, and the path to relief and prevention.
What is SI Joint Dysfunction?
It refers to pain arising from abnormal motion or alignment in the sacroiliac joints—either too much movement (hypermobility) or too little (hypomobility). This disrupts the crucial transfer of forces between your upper body and legs.
Common Causes (Etiology):
· Trauma: A sudden impact like a fall, car accident, or misstep.
· Repetitive Stress: Asymmetric activities (like golf, tennis), prolonged heavy lifting, or long-distance running.
· Biomechanical Issues: Leg length discrepancy, abnormal gait, or flat feet.
· Pregnancy & Childbirth: Hormones relax ligaments, and the physical strain can stress the joints.
· Degenerative Arthritis: Wear-and-tear on the joint.
· Spinal Surgery: Such as a lumbar fusion, which can increase stress on the SI joints.
Signs & Symptoms:
· Primary Complaint: Aching low back pain, typically below L5 vertebra, often felt on one side.
· Referred Pain: Pain can radiate to the buttock, groin, back of the thigh, or even the calf (mimicking sciatica).
· Aggravating Factors: Pain worsens with activities like climbing stairs, standing from a seated position, running, or prolonged sitting/standing.
· Specific Tenderness: Point tenderness directly over the PSIS (the dimples of the lower back).
· Joint Stiffness: Feeling of tightness or instability in the pelvis.
Therapeutic Treatment Approaches:
1. Physiotherapy & Therapeutic Massage:
· Manual Therapy: Skilled physiotherapists use specific mobilizations to correct joint alignment and restore normal motion.
· Soft Tissue Work:
Massage therapists target hypertonic muscles contributing to dysfunction—like the piriformis, gluteals, quadratus lumborum, and hip flexors—to reduce tension and spasm.
· Dry Needling: May be used to release trigger points in surrounding muscles.
2. Hydrotherapy:
· Hot Water Immersion/Sitz Baths: Applying moist heat (15-20 minutes) to the low back and pelvis can:
· Increase blood flow and promote relaxation.
· Reduce muscle guarding and stiffness.
· Provide temporary pain relief before exercises.
3. Core & Hip Strengthening & Stabilization Exercises: (Always start under professional guidance)
· Focus on: The deep core (Transversus Abdominis), gluteus medius/maximus, and hip stabilizers.
· Examples:
· Bridging: To activate glutes and hamstrings.
· Clamshells & Side-Lying Leg Lifts: For gluteus medius.
· Bird-Dog: For core and pelvic stability.
· Pelvic Tilts: To educate proper pelvic positioning.
· Proper Squat & Lunge Form: Learning to engage the right muscles.
Preventative Measures:
· Mind Your Mechanics:
Practice proper lifting techniques (lift with legs, keep objects close).
· Maintain Good Posture: Avoid standing with weight shifted to one leg. Use supportive seating.
· Stay Active: Regular, balanced exercise to maintain core and hip strength and flexibility.
· Footwear: Wear supportive shoes, especially if you have flat feet or a leg length discrepancy.
· Listen to Your Body: Don’t ignore persistent, one-sided low back pain. Early intervention is key.
· Cross-Train: Avoid repetitive, high-impact activities that load one side more than the other.
Key Takeaway:
SI Joint Dysfunction is a common but often overlooked cause of low back pain. It is treatable. A combination of professional care (physiotherapy/massage), targeted strengthening, and smart lifestyle habits can effectively manage pain, restore function, and prevent recurrence.
Disclaimer:
This is for health awareness only. If you are experiencing these symptoms, please consult a healthcare professional (like a doctor, physiotherapist, or chiropractor) for an accurate diagnosis and a personalized treatment plan.
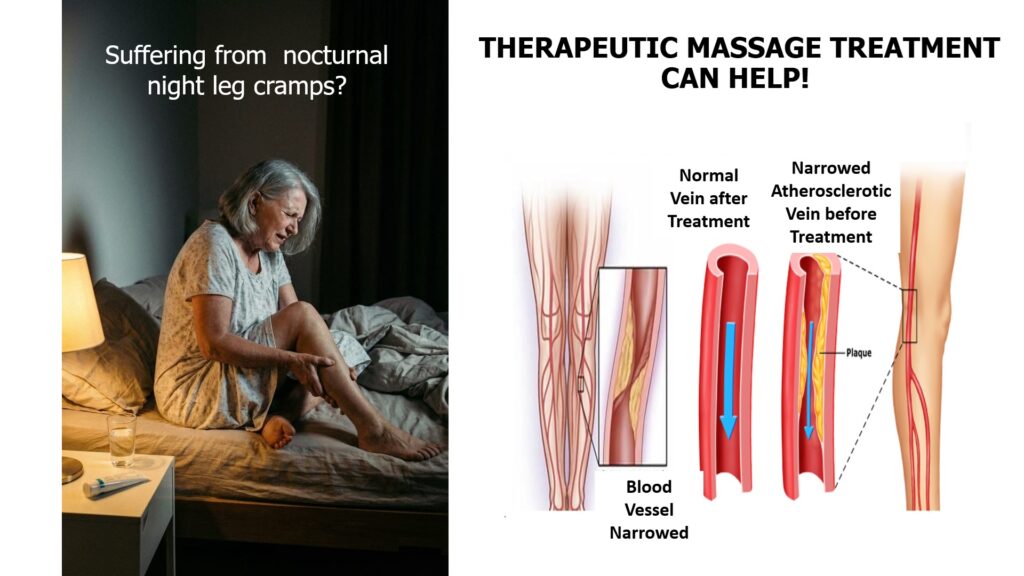
Are You Suffering from Night Leg Cramps?
Night Leg Cramps After 60: Restoring Restful Sleep with Therapeutic Touch and Warmth
If you’re over 60 and have been jolted awake by the sudden, excruciating grip of a leg cramp, you are far from alone. Nighttime leg cramps—those painful, involuntary contractions of the calf, foot, or thigh muscles—are a common, frustrating, and sleep-stealing complaint for many in their later years. While often harmless, their impact on quality of life is significant, leading to fatigue, anxiety about sleep, and next-day soreness.
The causes are multifaceted: natural muscle loss (sarcopenia), decreased circulation, medication side effects, dehydration, or electrolyte imbalances. While consulting a doctor is essential to rule out underlying conditions, many find that proactive, non-invasive supportive measures can offer profound relief. Among the most effective are regular therapeutic massage sessions and the simple, soothing power of hot water hydrotherapy.
The Knotty Problem: Why Cramps Strike at Night
At rest, circulation can slow. Muscles that may be subtly fatigued or dehydrated from the day’s activities seize up. The neural signals that regulate muscle contraction and relaxation can become slightly misfired. The result? A painful charley horse that pulls you from deep sleep. The goal of management isn’t just to stop the cramp in the moment, but to prevent its recurrence by addressing muscle tension, improving flexibility, and enhancing local blood flow.
The Healing Power of Therapeutic Massage
Think of therapeutic massage not as a luxury, but as targeted maintenance for your musculoskeletal system. For night cramps, it works on several levels:
1. Breaking the Cycle of Tension: Chronic, sub-conscious muscle tightness is a prime culprit. A skilled therapist can identify and release these hypertonic areas in the calves, hamstrings, and feet using techniques like effleurage (long, gliding strokes) and petrissage (kneading). This reduces the baseline tension that predisposes the muscle to cramp.
2. Enhancing Circulation: Massage acts as a passive pump, stimulating blood flow to bring fresh oxygen and nutrients to muscle tissues while flushing out metabolic waste products like lactic acid that can contribute to irritability.
3. Improving Flexibility and Range of Motion: Gentle, assisted stretching during a massage helps maintain and improve muscle elasticity. A more pliable, supple muscle is less likely to contract violently and painfully.
4. Neurological Calming: Massage down-regulates the nervous system, promoting relaxation and reducing the “hyper-excitability” of motor neurons that can trigger spasms.
For lasting benefit, consistency is key. Regular sessions (e.g., bi-weekly or monthly) create cumulative improvement in muscle health. It’s crucial to communicate with your massage therapist about the cramping issue so they can tailor the session. They can also teach you simple self-massage techniques for the calf—using your thumbs in a circular motion along the muscle or gently kneading the area—to use at home before bed.
The Soothing Embrace of Hot Water Hydrotherapy
Hydrotherapy—using water for therapeutic benefit—is one of the oldest and most accessible forms of pain relief. For night leg cramps, heat is the star.
How Warmth Works:
· Vasodilation: Warm water causes blood vessels to expand, dramatically increasing circulation to the submerged limbs. This delivers a healing surge of oxygenated blood.
· Muscle Relaxation: Heat has a direct soothing effect on muscle fibers, easing tightness and reducing the spasm potential.
· Pain Gate Theory: The sensation of warmth helps to “close the gate” on pain signals traveling to the brain, providing immediate subjective relief.
Practical Applications for Night Cramp Relief:
· Evening Epsom Salt Soak: Before bed, soak your feet and legs in a basin of warm (not hot) water mixed with Epsom salts (magnesium sulfate) for 15-20 minutes. The warmth relaxes the muscles, and the transdermal magnesium may help (though evidence is anecdotal, many swear by it). This ritual also primes your body and mind for sleep.
· Strategic Warm Compress: Apply a warm (not scalding) heating pad or a microwavable wrap to your calves while reading or watching TV in the evening. Focus on areas that typically cramp.
· Pre-Bedtime Shower: Direct the warm stream of water onto your calves and thighs for several minutes, massaging the muscles gently as you do.
· In-the-Moment Relief: When a cramp strikes, the fastest relief often comes from immediately applying heat. Keep a warm towel (heated in the microwave for a short time, tested for temperature) or a hydrocollator pack by the bed. Applying it to the knotted muscle can help it release faster than stretching alone.
Building Your Supportive Routine
Combine these approaches for a powerful defense:
1. Daily Prevention: Stay hydrated throughout the day. Perform gentle calf stretches before bed (like standing on a step and slowly lowering your heels). Consider a daily warm water soak.
2. Weekly Maintenance: Incorporate self-massage into your evening routine. Schedule regular therapeutic massage sessions for professional care.
3. Acute Intervention: Have a warm compress or bathrobe nearby at night for instant application during a cramp. Gently stretch the muscle after applying heat, when it is more relaxed.
A Final, Important Note
Always discuss persistent leg cramps with your healthcare provider to rule out causes like peripheral artery disease, nerve issues, or medication interactions. Once cleared, however, you have powerful, drug-free tools at your disposal.
Night leg cramps don’t have to be an inevitable sentence to poor sleep. By embracing the dual therapies of intentional therapeutic touch and the ancient comfort of hydrotherapy, you can soothe your muscles, calm your nerves, and reclaim your right to a peaceful, uninterrupted night’s rest. Your well-being is worth the investment.

